
Arthritis and degenerative joint disease are complex diseases affecting the joints. Because the symptoms are similar, many people think that the diseases are identical, but they are not. Arthritis and dry arthritis differ in their cause, the nature of their development, the area of damage, and the requirements for treatment are completely different.
Suppose two people see a doctor complaining about joint pain. One person is diagnosed with arthritis and the other has arthritis. While both patients sat in line, they had time to discuss a bit of their health problem.
It turns out their symptoms are very similar: the joints are sore, they don't bend / bend fully, they don't rest at night or during the day. Even the diagnoses are consonant, but they are still different. What is the difference between arthritis and osteoarthritis if both diseases affect joints?
What is Arthritis
Arthritis is an inflammatory disorder of the joint. It always precedes bone or cartilage tissue damage by a number of factors.
Biologically active substances are released from destroyed cells, causing an inflammatory response. The vessels in the damaged area dilate, filled with blood: thus, immune cells enter the joint tissue to fight off damaging factors.
At the same time, the fluid part of the blood leaves the vascular bed and develops edema, which limits the inflammatory area. This is the body's way of protecting itself from widespread harm from bacteria, foreign objects, and chemicals.
After the complete or partial removal of a pathogen, the healing mechanism begins. If the damage is minor, normal tissue function is restored. Deep defects are healed through a scar - an area of rough connective tissue that does not perform the normal function of the organ.
Arthritis goes through all of the following stages:
- change - damage;
- exudation - the formation of edema;
- proliferates - heals.
Reason
The causes are many, we will list the main ones:
- Streptococcal infection
- (tonsillitis, erythema) often leads to one complication - rheumatism;
- aggressive autoantibodies - proteins that the body produces against its own tissues; Such a situation occurs with a fault in the immune defense system, so she sees the joints as a foreign element to the body - rheumatoid arthritis;
- violation of purine metabolism leads to deposition of uric acid crystals in the joint - gout;
- allergic reactions may involve joint tissue with the development of an inflammatory reaction - allergic arthritis;
- long-term use of certain drugs that cause inflammation (isoniazid, D-penicillin, hydralazine, holes) - drug-induced arthritis; bacteria
- are introduced into the bloodstream or during surgery - septic arthritis;
- a viral or bacterial infection in any location that can indirectly affect joint tissue - this is reactive arthritis;
- acute trauma - recent injury (impact, bruising, cyst rupture).

Symptoms
This disease is characterized by an acute early stage, that is, in the context of complete health, a person suffers from severe pain in the joint. For autoimmune forms, symmetrical lesions of small joints are characteristic - between joints on the fingers, wrists, elbows.
Gout in most cases begins as evidence of arthritis between the thumb and foot. In bacterial and reactive arthritis, large joints are often affected on one side: the knee, hip, and sacrum (at the point of connection of the spine to the pelvis).
Rheumatoid arthritis develops on the basis of fever and general weakness, often preceded by angina. Severe inflammation of the bones, cartilage and synovial membrane can occur with fever, general intoxication: headache, weakness, loss of appetite.
Skin at the joint turns red and feels hotter than other areas. On the surface, it seems to be swollen and increase in volume. If the damage is only on one side, then a difference between a healthy limb and an diseased limb can be seen.
Limiting movement can lead to swelling and pain. If the joint cavity is slightly inflamed, then the activity is almost complete. With a pronounced pathological response, the entire synovial cavity can be filled with fluid - in this case, mobility is strongly restricted.
Treatment
Treatment is performed by a general practitioner, a rheumatologist or an trauma doctor - if the cause is mechanical damage. Therapy is aimed at eliminating irritants and suppressing inflammation.
For bacterial and reactive arthritis, antibiotics are required, for autoimmune diseases - cytostatics or glucocorticoids, for allergies - glucocorticoids and antihistamines.
Inflammatory fluid is removed with a special syringe or straw during arthroscopy. The joint is immobilized during the course of acute inflammation. After the patient is performed therapeutic exercises to restore joint mobility.
Doctor's advice
From the personal practice and work experience of colleagues - for any cause of arthritis, gelatin application has been shown to be effective. They are simple to make and cheap. The gauze should be folded into layers, length and width to fit the painful joint. Soak the folded gauze in hot water, squeeze, stretch. Pour a thin layer of gelatin on top, roll it up so that the filling looks like in the bag and doesn't spill over. Place on joint, wrap with the polyethylene bag above, fix with tape and / or tape. You can wear the pack for up to 3 hours, 2 times a day for 2 weeks. Usually the effect is felt on 4-5 days of use, but the treatment must be continued to achieve the desired results, if the treatment is interrupted, the pain will return.
What is joint disease
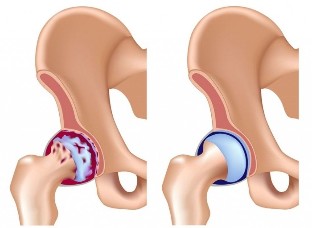
Arthritis (also known as osteoarthritis) is a degenerative-dystrophic disease. It is based on the depletion of joint cartilage, a slow and thinner recovery.
Simply put, the cartilage layer wears off faster than it can be regenerated. The joint surfaces are exposed. They are not as smooth as cartilage and rubbed together when moved. Bone plaques are partially destroyed, mild chronic inflammation develops.
As the disease progresses, bone spikes develop in the joints - a protective response to tissue against permanent damage. They interfere with the sliding of surfaces relative to each other, and joint mobility is impaired.
Osteoarthritis in most people begins to improve after 30-40 years, lasting for many years, with mild or moderate symptoms.
Osteoarthritis of the spine is often referred to as osteonecrosis.
Reason
There are factors that easily induce the development of pathology as a child and complicate its course:
- heavy physical activity among athletes;
- obesity;
- a history of joint injury; vascular disease
- ;
- sedentary lifestyle;
- violates the normal configuration of the joint, for example, with flat feet;
- long exposure to vibration;
- in women - hormonal imbalance or menopause.
Symptoms
Large joints on one side are most often affected: the knee, hip, and sacral joints. The disease begins not to be noticeable. Pain is rare at first and is associated with considerable exertion.
The discomfort goes away on the same day or for several days if the sick person is able to rest. As the disease progresses, pain intensity increases, even with normal everyday stress.
The mobility of the joint decreases and as a result the disease disappears. Movement in the affected limb causes severe pain. Osteoarthritis can be exacerbated by the type of arthritis - fluid builds up in the joint cavity, the upper skin turns red and hot. After the inflammatory response subsided, the course of the disease resumed as before.
Treatment
Arthritis is treated by trauma doctors, orthopedic physicians, sometimes surgeons. Therapy aims to restore cartilage metabolism, improve joint nutrition and eliminate inflammatory responses. Lifelong treatment, can be continuous or drug courses.
During severe periods, chondroprotectors are prescribed in the form of tablets and ointments, therapeutic exercises, massage. With exacerbations, chondroprotectors are administered intravenously or intramuscularly together with analgesics and anti-inflammatory drugs. The trauma doctor may inject a protective drug directly into the joint every few months.
The severe stage of the disease requires surgical intervention, in which the diseased joint is replaced by an artificial joint.
The difference between diseases
| Features | Arthritis | Arthritis |
| Causes of illness | Inflammation | Cartilage degeneration |
| Thread | Acute, chronic with exacerbations | Chronic|
| Pain | Intense from the start, more pronounced in the morning | The illness is weak at first, gradually increasing. It strengthens in the evening and after exertion |
| Motion | Need to "disband" - in the morning after bed, joints are least mobile | Tapering movement, not morning stiffness |
| Affected joints | The small joints of the hands and feet are symmetrically affected. The large ones are infected with bacteria | One or more large joints on different sides of the body |
| Blood test | Serious inflammatory changes in the general blood count, rheumatoid factor, C-reactive protein, antibodies against the pathogen | No property changes |
| X-rays | Varies by stage, osteoporosis - bone loss, cyst in the bone | Gradually changes, joint space deformation, bone spikes appear and grow out. |
| Basic treatment | Anti-inflammatory drugs | Chondroprotectors |
A feature that is similar in both diseases is a gradual progression and gradual loss of mobility. Autoimmune arthritis often manifests itself at a young age, when the patient is still wondering about his or her health.
It is important to remember that any joint pain that persists for a long time occurs under certain conditions - this is a serious reason to see a doctor. It is important to promptly diagnose the disease and initiate treatment to delay the development of the pathological process.





































